A regimen’s safety profile should support aging with HIV
People living with HIV (PLWH) currently require lifelong treatment through many stages of life
Aging with HIV
Prevalence of comorbidities in people living with HIV1
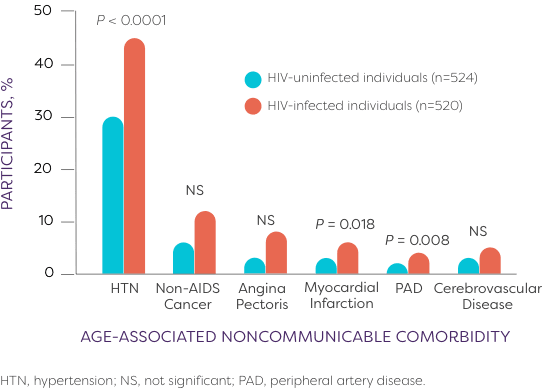
Age-associated noncommunicable comorbidities (AANCCs) in patients ≥45 years old (AGEhIV Study, 2010-2012)
The burden of aging-related diseases is significantly higher among persons with HIV than in the general population. Therefore, additional medical and social services may be required for management of both HIV and comorbid conditions.2
Older adults living with HIV in the US
In 2018, 51% of people in the US and dependent areas with diagnosed HIV were aged 50 years and older, though new HIV diagnoses continue to decline among this population.3
Antiretroviral therapy (ART) has increased life expectancy of individuals with HIV, and therefore, patients are living longer2
Aging patients with HIV face several potential health complications4
Older patients (>50 years of age) should be initiated on treatment as soon as possible after diagnosis because this population2:
- Experiences accelerated CD4 cell loss
- Has decreased immune recovery
- Is at increased risk of serious non-AIDS illnesses

As people age, they typically have more comorbidities, take more medications, and are more vulnerable to side effects—complicating management of their HIV.2
- Age-associated noncommunicable comorbidities (including hypertension, myocardial infarction, and peripheral artery disease) were numerically more prevalent among people living with HIV than HIV-uninfected controls in 20141
- Aging people with HIV often develop inflammation and cardiovascular, kidney, liver, bone, and neurologic disease5-7
- Potential side effects and drug-drug interactions for aging-associated comorbidities can further complicate ART management2
For illustrative purposes only. Not actual patient or physician.
Considerations to support long-term treatment success
A cross-functional approach to long-term medical care for people living with HIV is ideal. While the lifespan of people living with HIV has been extended since the advent of highly active antiretroviral therapy (HAART), other non-AIDS-related comorbidities persist in these patients.1,8
Therefore, people living with HIV should receive ongoing assessment for the following risks:
-
Persistent inflammation7
-
Neurocognitive considerations2
-
Alcohol and substance abuse, cognitive function, and psychosocial status assessed annually2,9
-
According to the DHHS guidelines, mental health disorders, including depression and anxiety, are a growing concern in both younger and aging patients with HIV2
-
Sleep habits, appetite, and suicidal/violent intent should be assessed during every visit2,9
-
Certain medications have adverse events related to the central nervous system2
-
-
Cardiovascular disease1
-
Immune activation and inflammation are believed to contribute to cardiovascular disease2
-
Cardiovascular disease is associated with adverse events from certain medications2
-
-
Drug-induced renal impairment and chronic kidney disease10,11
-
Hepatic considerations2
-
High-risk individuals should receive annual hepatitis B virus and hepatitis C virus screenings
-
-
Bone disease12
-
Age and gender should establish need for screening for fracture risk and BMD calculation
-
Weight gain in people living with HIV (PLWH)
-
For some patients, initiating ART may lead to weight gain, especially in patients with disease-related anorexia13
-
Attention to the maintenance of a healthy lifestyle, including diet and exercise, is an important aspect of HIV management. It is important to consider all factors that may contribute to weight gain for people living with HIV14,15
DHHS guidelines2
-
Assess a patient’s beliefs, perceptions, and expectations about the impact of taking ART on their health, including side effects2
-
Engaging in collaborative, problem-solving conversations regarding an individual’s questions or concerns about side effects may help improve their adherence to ART2
Discussions around treatment should take into account aging with HIV and the potential for comorbidities associated with HIV.2
ART, antiretroviral therapy; ARV, antiretroviral; BMD, bone mineral density; BMI, body mass index; CD4, cluster of differentiation 4; CrCl, creatinine clearance; CVD, cardiovascular disease; DHHS, US Department of Health and Human Services; INSTI, integrase strand transfer inhibitor; RNA, ribonucleic acid.
References:
- Schouten J, Wit F, Stolte I, et al. Cross-sectional comparison of the prevalence of age-associated comorbidities and their risk factors between HIV-infected and uninfected individuals: the AGEhIV cohort study. Clin Infect Dis. 2014;59(12):1787-1797.
- Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents with HIV. Department of Health and Human Services. Updated May 26, 2023. Accessed July 24, 2023. https://clinicalinfo.hiv.gov/sites/default/files/guidelines/documents/guidelines-adult-adolescent-arv.pdf
- Centers for Disease Control and Prevention. HIV and older Americans. Updated January 12, 2022. Accessed March 2, 2022. https://www.cdc.gov/hiv/group/age/olderamericans/index.html
- HIV.gov. Other health issues of special concern for people living with HIV. Published January 14, 2022. Accessed March 2, 2022. https://www.hiv.gov/hiv-basics/staying-in-hiv-care/other-related-health-issues/other-health-issues-of-special-concern-for-people-living-with-hiv
- HIV.gov. Aging with HIV. Updated May 17, 2021. Accessed May 26, 2022. https://www.hiv.gov/hiv-basics/living-well-with-hiv/taking-care-of-yourself/aging-with-hiv
- National Institutes of Health. HIV medicines and side effects. Accessed February 1, 2022. https://hivinfo.nih.gov/understanding-hiv/fact-sheets/hiv-medicines-and-side-effects
- Deeks S, Tracy R, Douek D. Systemic effects of inflammation on health during chronic HIV infection. Immunity. 2013;39(4):633-645.
- Marcus J, Chao C, Leyden W, et al. Narrowing the gap in life expectancy between HIV-infected and HIV-uninfected individuals with access to care. J Acquir Immune Defic Syndr. 2016;73(1):39-46.
- New York State Department of Health. Mental health screening. Published December 6, 2021. Accessed February 7, 2022. https://cdn.hivguidelines.org/wp-content/uploads/20210820091439/NYSDOH-AI-Mental-Health-Screening-Quick-Reference-Guide_8-20-21_HG.pdf
- Pazhayattil G, Shirali A. Drug-induced impairment of renal function. Int J Nephrol Renovasc Dis. 2014;7:457-468.
- Lucas G, Ross M, Stock P, et al. Clinical practice guideline for the management of chronic kidney disease in patients infected with HIV: 2014 update by the HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Dis. 2014;59(9):e96-e138.
- Brown T, Hoy J, Borderi M, et al. Recommendations for evaluation and management of bone disease in HIV. Clin Infect Dis. 2015;60(8):1242-1251.
- Saag M, Gandhi R, Hoy J, et al. Antiretroviral drugs for treatment and prevention of HIV infection in adults: recommendations of the International Antiviral Society–USA Panel. JAMA. 2020;324(16):1651-1669.
- Centers for Disease Control and Prevention. Healthy living. Published May 20, 2021. Accessed March 2, 2022. https://www.cdc.gov/hiv/basics/livingwithhiv/healthy-living.html
- Aidsmap.com. Weight gain and HIV treatment. Accessed March 28, 2022. https://www.aidsmap.com/about-hiv/weight-gain-and-hiv-treatment
